Every year in Germany, around seven boys are born with an incompletely formed urethra and urethral sphincter. These children often remain incontinent. ECRC researchers want to find out whether a stem cell transplant could help them. The trial has been awarded approximately €4.3 million in funding from the Federal Ministry of Education and Research (BMBF) and the Berlin Institute of Health (BIH) at Charité.
There are over 8000 known rare diseases, affecting more than 30 million people in Europe alone. Developing interventions for these mostly still untreatable diseases represents an important challenge for society and therefore to researchers. One such condition is epispadias, in which a developmental abnormality results in an abnormal position and splitting of the urethra and incomplete development of the urethral sphincter.
In Germany, only around seven boys and even fewer girls are born with this condition every year. It is associated with significant psychological stress, because although the externally visible malformation can be treated with surgery, in the case of the urethral sphincter this is unfortunately not so straightforward. "As a result, these children often suffer from lifelong incontinence, which causes considerable psychological stress for affected individuals and their families," says Professor Simone Spuler from the ECRC, a specialist in stem cell and muscle research. "So we considered how we could use our expertise to help them."
Muscle stem cells build new sphincter muscle
The research team led by Simone Spuler had developed a method that allowed them to isolate regeneration-capable muscle stem cells from muscle tissue. "We take a biopsy, a tissue sample, from the thigh and from this we isolate muscle stem cells. We then propagate these cells many times over and inject them directly into the defective area of the urethral sphincter muscle." In rats, this caused a new sphincter muscle to develop, one that was actually functional. Because their altered immune system tolerated human cells, the same result was achieved with human muscle stem cells.
"But despite these encouraging results, we couldn't begin a clinical trial right away with real patients because there are strict regulations in place," the researcher explains. "In humans, we're only allowed to use cells produced in a pharmaceutical process in line with good manufacturing practice, or GMP. Setting up a process like this is very complex." Cells produced under GMP conditions are first used in an animal model for preclinical safety testing.
Support from the USA – and from BIH
Regulatory authorities – in Germany the Paul Ehrlich Institute – stipulate that only specially accredited laboratories are permitted to carry out the animal experiments for a clinical trial. These labs must comply with good laboratory practice (GLP). In the search for a GLP lab that also had microsurgery capabilities – allowing the muscle stem cells to be transferred into the rat sphincter – the researchers found what they were looking for in the USA. "There was a lab that met the criteria about 300 km east of Chicago, in the heart of Michigan," says Simone Spuler. "To explain to the team there exactly what we had in mind, we had to make several trips to the USA. The preparations, the necessary familiarisation and the conducting of experiments were all extremely time-consuming and expensive. Without the support of the BIH Spark programme, we could never have done it!"
Turning research into health
BIH made €1 million available to Simone Spuler's muscle research team. "This is exactly in line with our purpose," explains Professor Christopher Baum, chairman of the Board of Directors of BIH and Chief Translational Research Officer of Charité. "We want to help researchers take their results from the lab to patients and in this way support clinical translation. This is how we turn research into health." Dr Tanja Rosenmund, the head of the BIH Spark programme, is also enthusiastic. "The reason the epispadias project is so exciting is that, if it succeeds, it will open up many other possibilities. Incontinence is a widespread problem, as is muscle weakness generally. So we hope that this funding will pave the way for many other studies."
Clinical trial with 21 boys
Now that the results in the USA have demonstrated that the transplanted muscle stem cells could prevent incontinence in rats and have also thoroughly confirmed the safety of the cell product, the clinical trial can go ahead. 21 boys aged between three and seventeen will receive treatment at the university hospitals in Ulm and Regensburg, where Professor Anne-Karoline Ebert and Professor Wolfgang Rösch lead centres for the bladder exstrophy-epispadias complex. The trial will take place on a placebo-controlled, randomised and double-blind basis. This means that a randomly selected five boys out of the group of 21 will be given a placebo (salt solution) instead of their own muscle stem cells. Neither the clinicians nor the patients will know which five these were until the end of the trial. "We have to do this to generate scientifically sound results," explains Spuler. "If the analysis of data shows that the children who received the cell injection are doing better than those who were given the placebo, those who didn't get the cell injection can of course be given it afterwards. This is possible because the isolated muscle stem cells can be stored without a problem by deep-freezing them."
The Federal Ministry of Education and Research was so impressed by the research proposal from Berlin that it made €3.3 million available to carry out the clinical trial. The first patient will be treated in a few months' time.
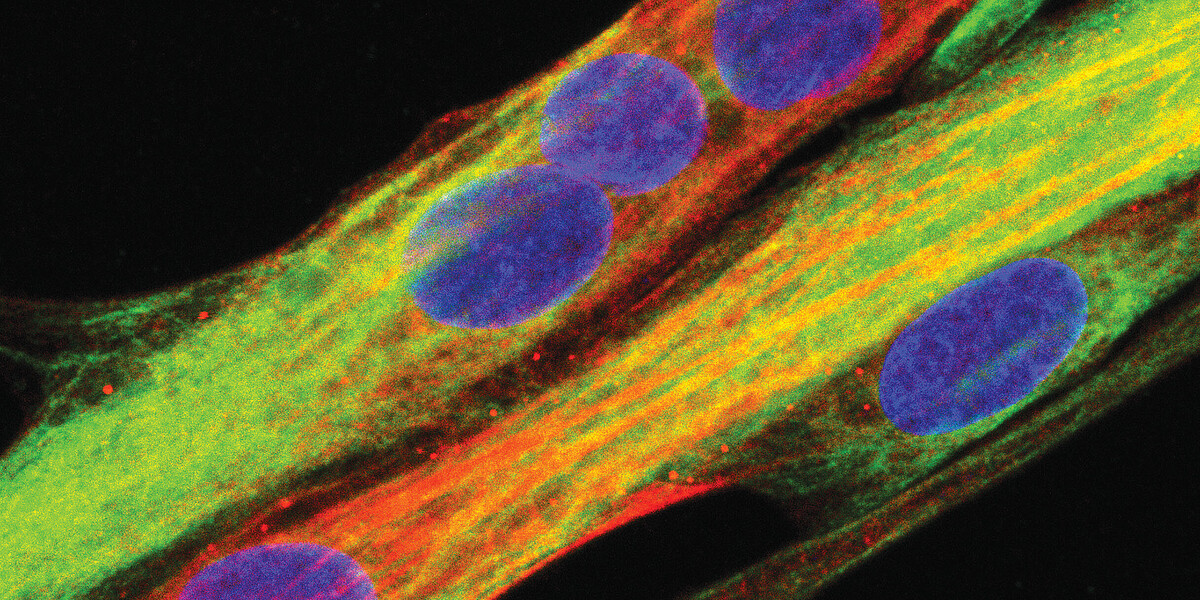
A photo of muscle cells is available on request.